Ph: 0493 519 744 | Email: info@osteophi.com.au

As an osteopath practicing on the Sunshine Coast I have treated many people with pain caused from disc issues. I have seen first-hand how painful, debilitating and scary that the process can be for patients. This blog will briefly discuss what an intervertebral disc is, how it can be injured, and how osteopathy can help manage pain and symptoms like sciatica.
Thank you to the anatomists who named the intervertebral disc. Sounds complicated but is actually pretty straight forward. It rests between two spinal vertebrae and is disc shaped.
I will spare you a detailed anatomy lesson but to understand how disc injuries happen it is important to get an understanding of the structures involved.
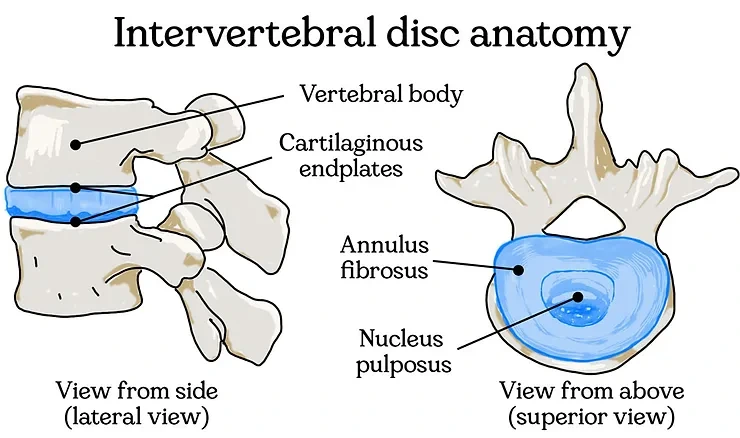
So, a disc’s outer layer is made of collagen, elastin fibres, water and magical proteoglycan proteins. This rigid outer layer is called ‘annulus fibrosus’ which poetically means fibrous ring.
The disc has a inner region they called the ‘nucleus pulposus’, this loosely translates to important-centre-fleshy-pulpy-thingy. Compared to the annulus fibrosus it has a different ratio of collagen, proteoglycan proteins and water and is therefore more soft and squishy.
Interestingly, the nucleus pulposus is a remnant part of the notochord which is a very important structure that helps our body develop as a foetus. The disc develop first and then the spinal vertebral segments either side of the discs!
The discs are sandwiched above and below by layer of cartilage and bone. Without explanation needed they are called ‘cartilaginous endplates’. They help anchor the discs structurally to the vertebrae and also help contain and distribute forces from disc material to the neighbouring vertebral body above and below.
Together these three parts work in concert offering unique properties of flexibility and stability for the disc to perform its function. The human spine is series of bones stacked vertically. Sweet, beautiful gravity compresses our spines towards the direction of the earth’s core. When we are standing upright against gravity the spine undergoes what is called vertical loading. Modelling of vertical loading on the disc is seen in picture A.
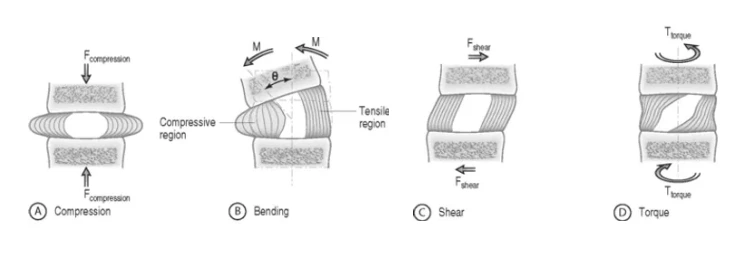
Structures of our spine are often loaded with vertical loading and multiple other vectors of loading due to movements of the spine and body. Modelling of these other vectors on the disc is seen pictures B, C and D.
When exposed to these forces the disc offers some important features of cushioning, stability, and flexibility.
The disc’s contents, it’s structural integrity, and height offer protection as we move. It is the disc’s ability to deform that helps transmit and disperse forces across structures of our spine and surrounding tissue.
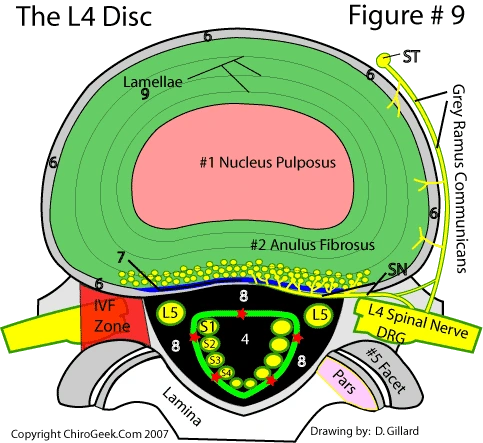
At a level between two vertebrae of the spine the discs help create space for exiting nerves from the spinal cord. These exiting nerves are important and very sensitive structures. They are the interface of sending signals to our body and receiving sensation from it. Without the structure of the disc not only would there be less movement permitted at each spinal level but there would be less space for the nerves.
Fun fact: did you know after waking, the average person is 1-2cm taller because of the increased water contents of the discs?
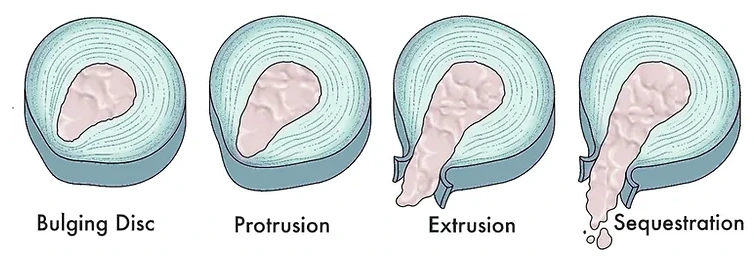
Technically, the term ‘disc bulge’ is one grade of how a disc can be mis-shaped. There are four disc bulge classification types.
A disc bulge is when there a ‘bulging out’ of inner contents of the nucleus pulposus. Signs of structural damage are seen in the inner region of the annulus fibrosus but the outer regions are still intact.
A disc protrusion is when there is a section of the nucleus pulposus bulging into the annulus fibrosus and the fiber ring is not interrupted.
A disc herniation or extrusion is when the annulus fibrosus is completely interrupted and fragments of the nucleus pulposus bulge out beyond the outline of the fiber ring.
A disc prolapse or sequestation is when fragments of nucleus pulposus and annulus fibrosus material detach from the main part of the disc.
Unfortunately, there are often many factors contributing to the mechanism of a disc injury, and the specific onset of it can be murky. Commonly, I see two modes of onset for a patient.
Sometimes, disc loading is repeatedly done for a long time before the disc is eventually aggravated. In these cases there is often a history of frequent (but lesser intensity) back pain episodes as a prelude to the increased aggravation event. Yes, even sitting in a certain position for time can compromise the structure of the discs and or sensitise the nerves associated with them.
Other times, there is a specific movement or trauma event that overloads the vertebral level and disc in question. Most common examples are like a sporting injury or trying to pick up something awkwardly, or too heavy. It can even be a simple unloaded movement that overloads one’s tissues – something like picking up a pencil. Don’t only consider the load that you are lifting but tissues involved going the overload on the segment leading up to that point.
It is important to note that in both cases the inflammation that a disc aggravation can cause is often delayed – this is confusing for a sufferer. There is often a large amount of pain that is felt and the delayed effect (often the next day) makes it harder to logically piece together the how and the why. As we lay still asleep, chemical signalling from injured disc cell tissues draws pro-inflammatory material from passing blood supply into and around the area – which now has a lower pressure in it because it is not vertically loaded and moving. Do you remember the modelling of disc loading from the picture earlier? The next day when someone who has aggravated their discs starts to move and load their discs it then causes pain. Like a rising tide, this inflammation process takes time to come up, and unfortunately it takes time to recede.
Consideration of a patient-specifics such as history and unique genetic makeup complicates contributing factors of inflammation.
Things such as; age, history of trauma, biomechanics, tissue capacity, exercise capacity, repeated vertical loading, flexing and twisting, nutrition and hydration, chronic pain, adequate sleep and rest, comorbidities and the makeup of an individual’s connective tissue all contribute. These things contribute to not only the capacity of the disc tissue but the individual’s internal inflammation levels along with their system’s ability to heal.
This certainly is an overview and for an individual the symptoms will vary. Disc research, like the rest of medicine certainly needs more research.
Did you know that other stressors in your life can contribute to an overall feeling of pain?
Although a type of disc bulge has structural deformation of the disc tissue, it doesn’t always have to directly push on, or pinch, the exiting spinal nerve to cause pain – even referred pain down the famous sciatic nerve. Depending on where the disc issue is, and what nerves are involved, you can have referred pain on your trunk, chest, abdomen, neck, back or down an arm or leg.
As mentioned previously, the pain often comes from inflammation. So you have to imagine that our tissues are bathed in (extracellular) fluid. When there is more inflammation in and around tissue, the nerves involved perceive more pain or have altered sensation.
These different kinds of sensations can be ie hot/cold, vibration, light touch, firm touch, muscle motor function, or information on where a joint is in time and space. It is this last idea of altered joint position sense that can sometimes make the spine or segment feel like it is “out” or misaligned. This altered joint feeling mostly comes from altered feedback from the nerve that supplies the spinal vertebral facet joint.
Cavet – I’m not disputing that there are no such things as structural ‘mal-alignment’ seen in spinal abnormalities such as; scoliosis (curvature of the spine), a forwards slippage (an anterolisthesis) or a backwards slippage (an retrolisthesis) of spinal segments. Just pointing out that inflammation can contribute to the changing of our sensation back from these spinal facet joints.
In the short term, the inflammation makes the associated nerves more sensitive to sending the signal of pain or an altered sensation – it lowers the threshold for the signal to be sent. This is a change from the nerves’ normal state as they otherwise would not send the signal. This phenomenon is still very painful and annoying but in its essence it is a protective mechanism – and if managed well, won’t last forever.
If an organism (human in this case) did not feel pain and continued to load inflamed tissues, more tissue irritation and inflammation would occur. This would feedback into the cycle and would likely lead to increased tissue damage at the site of injury.
In the long-term, if a spinal segment is re-injured again and again, inflammation can contribute to an accelerated degeneration of involved spinal structures. It is the same inflammatory cycle that also causes sensitisation of the nerves involved – both at the local level of the spine but also at higher levels in our brain where the involved nerve reports back to. Which highlights that staying consistent with managing the tissues of your spine as a preventative is a really important.
After a back pain episode has occurred and then subsided, remembering what the pain like can be a good thing. Although, an unpleasant memory it helps drive the need to be careful, work towards keeping the area strong and limber and knowing when to rest. Remembering the episode also helps stay focused on safely exposing your tissues to forces – which is the key of rehabilitation.
Fun fact: did you know the outer layer of the disc actually has nerves that supply it? Pictured below are the little nerves that supply the outer layers of the annulus fibrosus.
Having a game plan and seeking the expertise of a practitioner is indeed crucial when dealing with back injuries, including disc-related issues. While the typical time frame for recovery from back injuries is often around six weeks, it’s important to take proactive steps rather than simply waiting and hoping for the best outcome, especially if you have experienced previous episodes of back pain.
A skilled practitioner can assess and diagnose the injury, taking into account any clinical red flags that may indicate more severe underlying conditions. In such cases, appropriate referrals to specialists may be necessary.
Treatment provided by a practitioner can help alleviate symptoms, improve sleep quality, and facilitate a smoother return to work or daily activities. They can also assist in building confidence and provide structured guidance by gradually exposing your tissues to controlled loads. This approach, coupled with progressive exercises tailored to your capacity, can help prevent relapses and promote long-term recovery.
Additionally, practitioners can advocate for your case or coordinate care by writing letters to your employer or collaborating with other healthcare professionals. They may also recommend radiological imaging when necessary to further assess the extent of the injury.
Working closely with a practitioner allows for a tailored management plan specific to your case. They can help identify and modify contributing factors to reduce symptoms and improve overall management of your condition.
Having a management plan in place for lower back pain or recurrent episodes of back pain puts you in control of your own well-being and enables you to seek assistance when needed. It empowers you to take an active role in managing your pain and allows you to regain control over your daily activities and quality of life.
If you are experiencing pain, seek the help of a qualified health professional who can assist in addressing inflammation, guide your recovery, and help you get back to where you want to be.
Donec tristique sollicitudin sem et eleifend. Donec tristique sollicitudin sem et eleifend. Cras nec porttitor metus, in vulputate quam id ligula venenatis lacinia. Cras nec porttitor metus, in vulputate quam id ligula venenatis lacinia.
Lorem Ipsum is simply dummy text of the printing and typesetting industry. Lorem Ipsum has been the industry’s standard dummy text ever since the 1500s, when an unknown printer took a galley of type and scrambled it to make a type specimen book.